Mastitis, plugged ducts, and engorgement can cause unbearable pain and lead many women to stop breastfeeding before they’re ready. And mastitis can turn into a really serious condition – uncontrolled infection and breast abscess requiring surgery to resolve. So why is the guidance on these conditions so confusing and unhelpful?
The truth is, the guidance on mastitis has changed very recently to reflect new evidence on what’s actually happening in your body when you have these symptoms. It’s time to set the record straight so that you can handle this unexpected obstacle to your breastfeeding success with confidence.
What is mastitis?
Mastitis refers to any inflammation of the breast tissue including infectious mastitis, non-infectious (inflammatory) mastitis, and “plugged ducts”. And we now know that these conditions are exactly the same biological process along a spectrum. Treating the symptoms and underlying cause of mastitis spectrum conditions is actually exactly the same no matter which you have, and if you have typical engorgement in the first few days postpartum, the treatment is the same too!
What causes engorgement and mastitis?
In the first few days after delivery, your breasts may become painfully swollen as they fill with milk. This is extremely common and often confused with mastitis. In fact, it is a different condition most often caused by fluid retention from receiving IV fluids during labor in addition to the sudden volume of milk present.
Mastitis, on the other hand, is typically caused by some combination of oversupply and/or breast trauma. Both are usually a direct result of pumping – whether too much or with incorrect technique.
Techniques for relief
Breastfeed on demand
Nurse your baby on demand with a good latch every time. This is the best and fastest way to regulate your supply, relieve breast and nipple trauma, resolve inflammation, and heal the underlying cause of mastitis. For this to work effectively, it is absolutely critical to take a break from pumping while you’re working on relieving mastitis. It is safe to feed a baby from a breast affected by mastitis; the milk is not affected and the condition cannot make your baby sick.
Use anti-inflammatory techniques
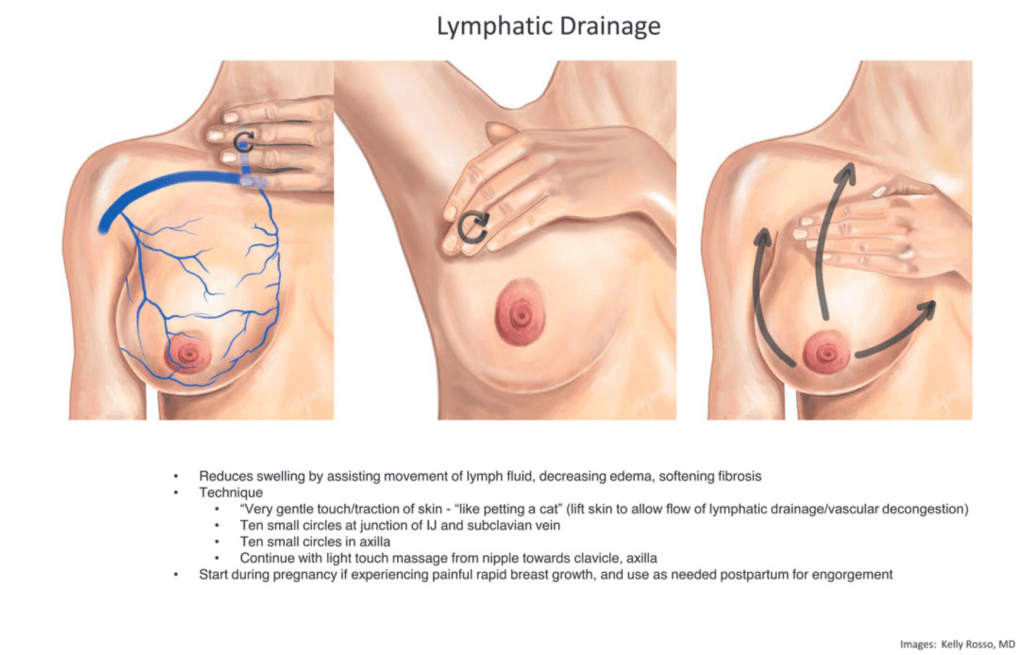
Although outdated advice recommended using deep massage, applying heat, and wearing a tight-fitting bra to relieve symptoms, we now know these techniques actually make mastitis worse. Instead, use gentle lymphatic drainage massage (see technique below), apply ice, and wear a well-fitting bra.
Source: Academy of Breastfeeding Medicine Protocol #36 The Mastitis Spectrum
Ask your doctor about medications and supplements
Ibuprofen is an over-the-counter NSAID medication that is generally considered safe for breastfeeding and can relieve pain and inflammation. Ask your doctor if it is safe for you to take ibuprofen for your condition. Additionally, some studies show that sunflower or soy lecithin can be effective in relieving mastitis symptoms.
When to seek help
Mastitis can progress into a dangerous condition if it doesn’t resolve quickly, so it’s important to get help from your IBCLC and physician as soon as you need it.
If you have mastitis and a nipple wound
A nipple wound could indicate a poor latch, so seek help from an IBCLC immediately to improve the latch first.
If you have mastitis while pump-dependent
If you have a baby who cannot breastfeed well because of prematurity or another medical condition, you may not be able to avoid pumping entirely. If your mastitis occurs at a time when you can’t avoid pumping, work with an IBCLC to determine the best way to adjust your pump settings to improve your condition. If your baby does breastfeed well but you’re usually pumping while away at work, consider taking a sick day or two to resolve your mastitis before going back to the pump.
If your mastitis interferes with breastfeeding
Mastitis may cause such severe pain or extreme inflammation that comfortable breastfeeding is actually not possible. If this happens to you, reach out to an IBCLC immediately to get feeding back on track.
If your symptoms don’t resolve
A fever can be normal with inflammatory mastitis, but if your fever does not resolve within 24 hours of treatment, contact your doctor right away as you may have an infection requiring antibiotics. Also contact your doctor if your mastitis symptoms other than fever don’t resolve at all after 48 hours. And if you have mastitis multiple time, it’s a great time to have a chat with your IBCLC about why that might be the case.
Summary
Mastitis, plugged ducts, and engorgement are painful and scary, but they don’t need to happen to you! Using these techniques will help you avoid these conditions or resolve them quickly when they occur.

Leave a comment